August 7, 2015
Who should be accountable for NEEDLESS job loss due to medical conditions?
Who do you think should be held accountable when workers needlessly lose their jobs because a newly-acquired or changed health condition or disability?
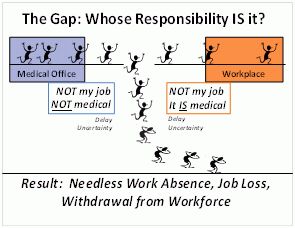
Right now, none of the professional participants who play front-line roles in the stay-at-work/return-to-work process feels a responsibility to prevent unnecessary job loss. Doctors, employers, insurance companies, lawyers and so on simply think it’s a shame when it happens — if they are even aware of it. Unnecessary job loss is being viewed as a private tragedy rather than a sentinel indicator of service and system failure. A lot more sunshine is needed to illuminate this dark corner.
Even though OSHA ensures that employers record the number of work-related injuries, lost work-days and deaths, there is no requirement that they record job loss. Why isn’t it being tracked? It will almost always be a much worse consequence than the injury itself. Job loss, especially in someone who was previously healthy but now has some degree of impairment, can be DEVASTATING. Few people are prepared to deal with this double- barreled challenge. For the unlucky ones, this means losing their footing in the world of work forever.
We do not even KNOW how many people lose their jobs as the result of work-related injuries much less personal health conditions — and how many fail to find new jobs. I personally don’t think it matters what the cause of the health condition is.
These days, more than a HALF of the people entering the Social Security Disability Insurance program are doing so because of adverse secondary consequences of common health conditions like back pain, joint pain, anxiety, and depression. But notice this: there are literally MILLIONS of people who keep working DESPITE back pain, joint pain, anxiety and depression. These conditions should NOT be forcing people into a bleak future of on-going worklessness, especially because unemployment and poverty will WORSEN their health and well-being — and that of their families.
Needless job loss can occur because of decisions that doctors and employers make as well as decisions made by workers, their lawyers, and insurance companies. Anyone who COULD have actively supported a worker in staying at work but DIDN’T plays a part in unnecessary job loss. Doctors may thoughtlessly select treatments that worsen instead of improve function, or impose work restrictions that “over-limit” someone who COULD actually perform their job. Employers may refuse to make temporary adjustments that WOULD permit recovery “on the job” — and as a result workers sit home and begin to believe they really are “too disabled to work”. Employers can refuse to engage in a real problem-solving discussion with workers that WOULD have let them come back to work with a very minor modification. Employers can neglect to ask for help from a return-to-work expert who COULD have told them about a $200 piece of equipment or work process alteration that WOULD have made it possible for the worker to keep doing her regular job. Insurers COULD routinely (instead of occasionally) make career counseling and job finding services available to workers who appear headed for job loss or have already been terminated. Etc. Etc.
So, who DO you think should be held accountable for job loss in those situations? You and I as taxpayers are going to pay benefits for the rest of these people’s lives if they end up on SSDI because the right things didn’t happen. Less than 1% of SSDI beneficiaries ever come back off the rolls.
Here’s a place to see and comment on my DRAFT recommendations for what the government can do to create a lot more visibility for unnecessary job loss due to acquired health conditions and disabilities. You can also contribute your own ideas on this matter at: http://workashealthoutcome.epolicyworks.org/