November 19, 2015
Early EVENTS influence outcomes: You have power to make good things happen!
Few people realize how important early EVENTS are in determining the eventual outcome of a work disruption due to a health problem, particularly the most common kinds of conditions: low back pain and other kinds of muscle and joint sprains and strains, depression, and anxiety.
Let’s call this a poor outcome: a failed medical recovery that results in over-impairment and excessive “disability” accompanied by work absence and loss of employment that could have been avoided. And let’s call this a good outcome: the fullest possible medical recovery with the least possible physical or mental impairment and the smallest possible impact on the rhythm of everyday life, including minimal lost work time and continued employment. Do you agree?
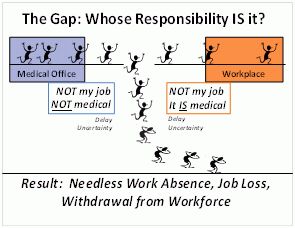
Here’s the exciting “so what” about this news that EVENTS influence outcomes: all three of the professionals who respond to an individual CAN influence what some of those EVENTS are going to be. Those three professionals are: the treating doctor, the workplace supervisor, and the benefit claims handler. This news means that each of them actually has some POWER to nudge things in a good or bad direction!!
See below for a brief description of why early events are so important, and how the experience of people destined for lucky or unlucky outcomes differs. In fact, these ideas are some of the main concepts of the work disability prevention model. (NOTE: The scientific articles that support the evidence-based concepts are briefly noted in parentheses. Their full literature citations appear in the list of References in our report that recommends the establishment of a nationwide Health & Work Service.)
When a working person’s life is disrupted by a new or changed illness or injury, the first few days and weeks after onset are an especially critical period. The likelihood of a good long-term outcome is being influenced, either favorably or unfavorably, by some simple things that either do or do not happen during that interval (Bowling 2000; Cornelius et al. 2011; Franklin et al. 2013; Loisel and Anema 2013; Nicholas et al. 2011; Shaw et al. 2013; Waddell and Burton 2004; Waddell, Burton, and Main 2001). It is the optimal window of opportunity to improve outcomes by simultaneously attending to the worker’s basic needs and concerns (Shaw et al. 2013) as well as by coordinating the medical, functional restoration, and occupational aspects of the situation in a coordinated fashion (Wickizer et al. 2011).
The way the episode unfolds over time in all dimensions — biological, psychological, social, and economic — can have a big impact on the outcome. Events that occur can either mitigate or aggravate existing risk factors in the situation, leading to better or worse outcomes. There are usually many opportunities to actively influence the course of events immediately after onset of a health problem (and many fewer opportunities later on), but today there are few resources devoted to finding and exercising these opportunities. Most of the current attempts to steer situations to a better outcome are made long after the best opportunities have passed by.
The best opportunity for basic intervention appears to last about 12 weeks or three months (DeWitt 1995; Franklin et al. 2013; Hashemi et al. 1997; Johnson and Fry 2002; Loisel and Anema 2013; Turner et al. 2008) although some data shows it ending by 6 months (Rumack 1987; Waddell and Burton 2004). A modest set of simple services —that embody an immediate, systematic, pro-active, integrated, and multidimensional approach — can mitigate the potentially destructive impact of common injuries, illnesses, and chronic conditions on quality of life among the working population (Burton et al. 2013; Hill et al. 2010; Iles, Wyatt, and Pransky 2012; Kendall et al. 2009; Lagerveld et al. 2012; Loisel and Anema 2013; McLaren, Reville, and Seabury 2010; Mitchell 2012; Nicholas et al. 2011; Shaw et al. 2013; Sullivan et al. 2005; Turner et al. 2008; Waddell and Burton 2004; Wickizer et al. 2011).
This new approach will allow people to avoid the kind of adverse secondary consequences of medical conditions that they too often experience today (Institute of Medicine 2001; Dartmouth 2008; Franklin and Mueller 2015). Those consequences are not usually obvious until months or years later, after unfortunate things have happened. The unlucky ones have received sub-optimal health care, been left with undertreated or iatrogenic impairment, become dependent on opioids, found themselves socially isolated, lost their jobs, withdrawn from the workforce, lost economic independence, and ended up on long-term disability benefits programs or SSDI in order to survive (Darlow 2011; Franklin et al. 2008; Franklin et al. 2014; Franklin and Mueller 2015; Habeck, Hunt, and VanTol 1998; Nguyen et al.)
CLARIFYING KEY TERMS
Figuring out where the opportunity to improve outcomes actually lies will be easier if we first clarify some terms that are often used carelessly or that mean different things to various audiences.
Work Disability vs. Disability
In the world of employment and commercial insurance, the word “disability” is carelessly used. In this world, the correct term is often “work disability” –which means absence from or lack of work attributed to a health condition.
According to the ADA, disabilities are impairments affecting major life functions (such as work). Having a disability need not result in work disability. This is a core concept embodied in the Americans with Disabilities Act. Similarly, having symptoms or a diagnosis need not (and usually does not) result in work disability.
Medical Recovery vs. Functional Restoration
Medical recovery refers to the resolution (disappearance or remission) of the underlying pathological process. Functional restoration refers to reestablishing the usual rhythm of participation in everyday life including the ability to go about one’s regular daily business: performing necessary tasks and enjoyable activities at home and work, and participating fully in society. Functional restoration often accompanies medical recovery, but not always. Even when medical recovery is not possible, restoration of function often is. In some cases, it may require separate and specific professional attention. Functional restoration may include rehabilitation (broadly defined), the successful use of assistive technology, adaptive equipment, and/or reasonable accommodation in the workplace.
Anticipatory programs that ensure the right things happen from the start and include early identification of those needing extra support are the simplest and most effective way to prevent later adverse secondary consequences of these conditions. A professional needs to provide the following services throughout the immediate response period (which typically ends with stable RTW or 12 weeks post onset). These services are not generally available today, especially to lower-wage workers and those who work for small firms:
- oversee and champion the affected individual’s stay-at-work and return-to-work (SAW/RTW) process until it is successful.
- conduct a quick initial assessment and planning session that considers the individual’s entire situation, screens for known risks for poor outcomes, helps the individual and/or employer make a SAW/RTW plan and support them in carrying it out;
- drive towards the best outcome by:
— expediting and coordinating external medical, rehabilitative and other kinds of helping services, including referrals for specialized services as needed to address remediable obstacles in a variety of life domains;
— facilitating communications among all involved parties, ensuring they get the information they need so everyone has a shared picture of the situation and the goal;
— taking a problem-solving approach with affected individuals, treating physicians, employers, and payers.
If RTW has not occurred by the time the 12 week period has ended, that should trigger a hand-off to another professional with broader expertise for a deeper assessment which is likely to reveal the need for a different strategy, revised goals, a new approach, or the involvement of other disciplines.