Something called “shared medical decision-making” increases patient satisfaction while reducing utilization of elective procedures that are invasive, risky, of questionable value — and often high cost. But it is rarely used today outside large health plans.
Do you know how shared medical decision-making (SMDM) differs from “informed consent”? I didn’t until I attended a presentation by Ben Moulton from the Informed Medical Decisions Foundation. In brief, informed consent is a legal process that is supposed to protect patients and promote patient autonomy. You’re probably familiar with it. You get a form to read a minute before the doctor walks in to talk at you for a few minutes about risks and benefits of your up-coming test, procedure or surgery. Then you sign the form after barely glancing at all the legalese. In contrast, SMDM is a structured process by which a patient and a clinician share information with each other in a two-way exploratory conversation that prepares the patient to make a truly informed decision. The INSTANT I learned about SMDM, I became an ardent fan.
(Please forgive the acronyms. We have been doing a project with the military. They constantly use acronyms in the interest of brevity. I now find myself making an acronym out of EVERY multi-syllabic or multi-word term. Here’s the latest one I learned: BLUF which means “bottom line up front”. In other words, instead of beating around the bush, the point of the memo or report is right here at the start!)
So here’s the BLUF: Since the superiority of SMDM is now well-established among healthcare researchers and legal scholars, and many articles have documented its benefits to patients, to healthcare professionals, and in some cases to health payers, why isn’t it in widespread use every day and everywhere? As soon as I heard SMDM existed, I began to wonder about what’s getting in the way of constant use? I bet a combination of conflict of interest and pesky not-so-little logistical details like the lack of vendors, undeveloped operational mechanisms, and lack of fair payment for effort are the main reasons why. And of course, a preference for costs later rather than costs today. We gotta find a way around those obstacles!
BACKGROUND:
Ten years ago, a landmark article appeared that distinguished between informed consent and SMDM — then made a persuasive case for the latter. Here’s the full citation: King, Jaime S. and Moulton, Benjamin, Rethinking Informed Consent: The Case for Shared Medical Decision-Making. American Journal of Law and Medicine, Vol. 32, pp. 429-501, 2006.
First the authors described the two prevailing types of legal definitions for informed consent. They wrote: “Currently, the states are almost evenly split between two types of standards for informed consent – the physician-based standard, effective in 25 states, and the patient-based standard, effective in 23 states and the District of Columbia. Physician-based standards generally require physicians to inform a patient of the risks, benefits and alternatives to a treatment in the same manner that a ‘reasonably prudent practitioner’ in the field would. On the other hand, patient-based standards hold physicians responsible for providing patients with all information on the risks, benefits and alternatives to a treatment that a ‘reasonable patient’ would attach significance to in making a treatment decision.”
The crux of the problem: About one third of the time, the prevailing standard of care does not require the physician to do the treatment (for example, the surgery is not the only treatment available, or is not required to save the patient’s life). In that third of cases, in which the treatment or procedure is referred to as “elective”, the intended outcome of the surgery is basically improved quality of life. Thus, the decision whether to go ahead with the treatment really should depend largely on the values and preferences of the patient. However, patients vary widely in how much information they want, their appetite for risk, their tolerance for various side effects and possible poor outcomes, and their confidence in their own decision-making ability. Many of them will not feel prepared to make a good decision no matter how much information they get; they want guidance or an out and out recommendation from their doctor. Without knowing the patient’s preferences and values, physicians are not able to give advice about treatment decisions tailored to the patient’s personal situation — and may inappropriately bias the discussion of alternative plans.
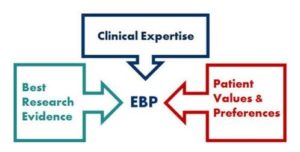
Then the authors defined SMDM: “a process in which the physician shares with the patient all relevant risk and benefit information on all treatment alternatives and the patient shares with the physician all relevant personal information that might make one treatment or side effect more or less tolerable than others. Then, both parties use this information to come to a mutual medical decision.” They also said SMDM must occur BEFORE the patient can give truly informed consent.
Here’s another problem: Many physicians have trouble talking in lay language; they tend to use big words and medical jargon. And because medical visits are stressful, patients have trouble remembering the things the doctor tells them. Moreover, most physicians do not have comparative factual data at hand about likelihood of success and specific side effects for the various treatment alternatives. This has led to the development of decision aids – pamphlets, booklets and videos for patients that summarize information about procedures and treatments, their likelihood of success, what it is like to live with potential side effects and poor outcomes, and so on, all written in simple everyday language. Both the Foundation and its partner Healthwise have produced many of them.
Finally, the authors asserted that despite the “bureaucratic headaches, the enormous expenditure of financial and human resources, and the need for state by state adoption of new informed consent laws, the long-term benefits of shared decision-making and the use of evidence based decision aids to promote patient understanding of medical information to arrive at informed medical decision making far outweigh the costs for both patients and physicians.”
MY SIMPLISTIC ANALYSIS OF THE REASONS FOR LOW USE
Conflict of interest:
Some (or many) surgeons and interventionists of various kinds earn their living by delivering expensive services – and usually have convinced themselves believe those services are the best thing for the patient. They often work for healthcare delivery organizations that want to drive revenue up – not down. The whole team has a vested interest in making sure the patient says “yes” and understandably has less commitment to spending valuable time helping patients say “no thank you” to the operation or the treatment.
My question is: How can we get around this obstacle? Why can’t managed care companies or health/disability/workers’ comp payers find qualified third party vendors who can engage patients in shared medical decision-making conversations when the treating physician can’t – or doesn’t want to? The company Health Dialog does that – but last time I talked with them, they are only set up for bulk sales to healthplans. I haven’t yet run across an organization that will do onesie and twosie shared medical decision conversations on request. In workers’ compensation and disability benefits programs, that option is the only way this will fly.
Scarcity and cost of materials, logistics, and lack of delivery mechanisms:
1. Materials to educate and prepare the patient for shared medical decision-making are available only for a limited number of procedures. It takes time and expertise to prepare them, and since they are based on the latest scientific evidence, they must constantly be updated. For example, when I looked last, the Foundation had no package for spine fusion surgery, though they did have them for laminectomy and spine MRI.
2. Medical offices that buy the materials used to educate and prepare the patient for a shared medical decision-making conversation can’t bill for the cost of the materials. There is no CPT billing code expressly designed for it, and if the provider bills under a similar-appearing code, it often won’t be paid.
3. Physicians who conduct “real” shared decision-making conversations in their office aren’t paid for the time. There is no CPT billing code expressly designed for it, and if the provider bills under another code, it often won’t be paid.
4. Medical delivery organizations that have especially trained staff on hand to conduct these conversations can’t bill for the time they would spend doing it. Non-physicians can’t bill health payers for the time they spent on these conversations. There is no billing code expressly designed for this service, and if the provider bills under another CPT code, it usually won’t be paid.
GOTTA FIND A WAY TO MAKE THIS WORK
Many studies have shown increased patient satisfaction when SMDM occurs. In addition, Group Health of Oregon reduced healthcare costs by 40% by putting SMDM in place throughout their group practice HMO. (They didn’t have to worry about getting paid for doing it because Group Health is a prepaid health plan that employs its own physicians. Increasing patient satisfaction strengthens their business, and any dollars they save stay in house)
Those of us who contract with vendors and operate provider payment mechanisms really ought to get ourselves in gear to remove the barriers to widespread adoption of SMDM. Drs. Ian Hargreaves and Victor Montori from the Mayo Clinic summarized the situation in an article in Health Affairs entitled “Shared Decision Making: The Need For Patient-Clinician Conversation, Not Just Information,” They wrote: “The patient and clinician must jointly create a course of action that is best for the individual patient and his or her family. The larger need in evidence-informed shared decision making is for a patient-clinician interaction that offers conversation, not just information, and care, not just choice.”
Like this:
Like Loading...