August 14, 2015
Interview with Praxis Partners founding member: Chris Brigham, MD
From time to time I will be interviewing members of the Praxis Partners Consortium, and encouraging them to tell us what they are up to. This first interview is with one of the founders of Praxis, Christopher Brigham, MD. He is an internationally recognized thought leader on human potential, impairment, and disability. More biographical information appears below the interview.
JC: Please begin by telling us, Dr. Brigham, why you decided to join the group that founded the Praxis Partners Consortium?
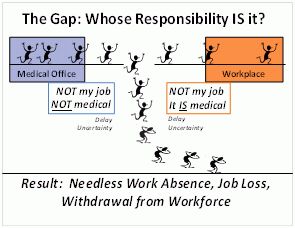
There appears to be an underlying philosophy that we share. Contemporary society needlessly traps so many into being injured and ill, and ultimately to being disabled. Our health care and disability “systems” are broken and badly in need of repair – ultimately resulting in poor health outcomes and needless disability. We have fragmented components that often focus on what is most beneficial for the providers and others in the industry, rather the individual. Incentives, perceptions and motivations often make all the difference in our health and in our lives. Societally-defined “disability” often fails to recognize the dynamics of human potential and the benefits of an active life. Each day countless individuals experience needless disability and poor health outcomes that are preventable. As a nation, employers, and insurers we confront ever-increasing costs. This is a tragedy for each of us, our families and our society. The United States leads the world in health care costs, however we are not healthier nor do we live longer. We need to share this information widely. It is together that we will create change, starting by creating awareness.
JC: Can you tell us a bit about the book that you and Henry Bennett recently published entitled Living Abled & Healthy: Your Guide to Injury & Illness Recovery.
Living Abled & Healthy is a guide for all of us on taking charge during injury or illness rather than allowing others to take charge of us. It is linked with a website, www.livingabled.com, which provides web-based resources.
JC: What inspired you to write Living Abled & Healthy?
For over three decades, as a clinician and as a researcher focusing on health and disability issues, I have pondered:
• Why do people with similar problems, even when they receive the same care, sometimes have dramatically different outcomes?
• What defines disability and how may it be prevented?
• How do compensation systems, healthcare professionals, and our own actions contribute to our health or disability?
• How are we best able to experience joyful and productive lives?
I had encountered too many people who were experiencing needlessly diminished lives, while at the same time I was inspired by others who were living exceptional lives despite significant injury and illness. I have also been appalled by others who misuse trusting individuals for personal financial gain. I realized I could have more impact by writing and sharing my insights with others, and my co-author Henry Bennett supported me in making that possible.
JC: Can you share some tips from your book on how to recover from injury or illness?
Here are ten core principles that we have found most helpful in recovering from injury or illness
1. Taking control of our life and health
We all need to take and keep control of our lives, including our health. When we have a health challenge, we need to identify our best resources and then take action. No one else may be allowed to dictate our lives. Our moments of doubt must not be exploited by others.
2. Staying positive
A positive attitude helps us to focus on our strengths, understand but ignore our weaknesses, and move on with our lives. When we change our thinking and our beliefs, we change our lives.
3. Partnering with quality healthcare providers practicing evidence-based and data-driven medicine
When doctors offer us a conclusion or recommendation—whether about our diagnosis, what caused our problem, or ordering tests or treatments—we want to believe they have solid reasons. We want our medical care to be based on the best available evidence, identified by scientific method, for clinical decision-making. This process is known as “evidence-based medicine.”
4. Approaching health problems from a “biopsychosocial” perspective
To better understand injury, illness, and disability, we embrace a “biopsychosocial” approach including biological, psychological, and social elements. Physical illnesses affect all of who we are—including our minds and spirits. Our mind-body connections are surprisingly strong. Physical, social, and work environments all affect health.
5. Weighing the risks and benefits of testing and treatment
All testing and treatment is associated with risks and possible benefits. We need to discern what is best for us. When doctors recommend testing or treatment we need to ask what the risks and benefits may be.
6.Focusing on a healthy body, mind, and spirit
Health encompasses our bodies, minds and spirits—they all relate. What goes on in our minds—attitudes, beliefs, perceptions, and resiliency—significantly affects what happens in our bodies. Thoughts affect bodies at least as much as bodies affect thoughts. Maintaining a strong spirit gives us purpose. Mastering these concepts helps us master our lives.
7. Choosing smart lifestyles including exercise, diet, and health habits
We can eat right, stay physically fit, maintain an appropriate weight, do our best to sleep well, not smoke, and not abuse alcohol and/or other drugs. Our choices are important factors in whether or not we stay healthy. We need to be honest with ourselves. We can make healthy choices.
8. Weighing the risks and benefits of involving lawyers
Sometimes we need the assistance of lawyers, other times we do not. Involvement with lawyers may complicate our lives and result in poorer outcomes—for us. If our situation requires a lawyer, we need to discern how to select the best lawyer and make sure they are working for us.
9. Cooperating with other healthcare participants and avoiding unnecessary conflict
We should choose our healthcare participants wisely and then maximize the value we obtain from them. This requires careful planning.
10. Continuing with our jobs, if at all possible
Work is, in general, good for our health and well-being. Our work often helps us to establish who we are, our identities, and our status. Work provides structure and gives us a reason—a need—to get up daily. Not working places us at greater risk of poorer physical and mental health, long-standing illnesses, psychological distress, increased use of healthcare resources, and death.
Where can people get more information?
At the website of www.livingabled.com and the book is available on Amazon, among many other sources.
Biographical information. Chris Brigham received a Masters of Medical Science from Rutgers Medical School, an MD from Washington University in St. Louis and did post-graduate training at the Eastern Maine Medical Center in Bangor, Maine. He is board-certified in occupational medicine, highly credentialed, has edited and co-authored several books, and written over two hundred peer-reviewed articles. He is the Editor of the AMA Guides Newsletter and Senior Contributing Editor for the AMA Guides to the Evaluation of Permanent Impairment, Sixth Edition. He is committed to working with others in the application of evidence-based medicine and best practices to promote function and avoid needless disability. Dr. Brigham is also an accomplished professional speaker. He is passionate about creating change that will:
• empower individuals to live productive lives and
• reduce human and financial costs associated with disabling.