January 5, 2017
Why Public-Private Collaboration Is Necessary to Prevent Work Disability
My goal now is to raise awareness about the need for concerted governmental, philanthropic, and private sector action to find better ways to support the millions of workers who lose their livelihoods each year due to injury or illness. In many cases, this outcome could have been prevented. And in the New World under President Trump, it will probably be more important than ever to make sure that people get the help they need to KEEP earning a living and STAY in the workforce.
You may be wondering … why work disability is a problem? Let’s start with the basics. As a practical matter, we already know that lack of work is bad for people and for communities. Just think about the many millions of dollars the government spends to create jobs and reduce unemployment! But now, formal research has started confirming how harmful worklessness really is for adults — documenting the consequences for their physical and mental health as well as for their marital, family, social and economic well-being.
Since that’s so obvious…. let’s agree that preserving people’s ability to function and work should be a fundamental purpose of health care services. Successfully doing so should be seen as an especially valuable health care outcome, second only to preserving life, limb, and essential bodily functions. And the failure to do so should be called a poor outcome.
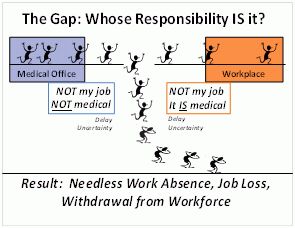
Today’s reality is … that whether or not a person with an newly-acquired medical condition is able to function and work afterwards is not even counted as a health outcome! And there are gaps in our social fabric that are actually creating job loss and work disability.
Here’s one big example of a gap: … None of the three professionals typically responding to workers who are dealing with life disruption due to injury or illness feel any responsibility for actively supporting the workers to keep their jobs or find new ones if necessary. That includes health care professionals, employers, and benefits administrators. Occasionally, some of these professionals actually advise against work — not realizing the consequences, of course. The workers are left to fend for themselves; some lack the confidence or skills to do so successfully. We need better public policy, stronger governmental efforts, and more support from the private sector in order to prevent this needless work disability.
Do you realize… that roughly half of the people now receiving Social Security Disability Insurance (SSDI) and other prolonged disability benefits started out with very common health problems like back pain, depression, and anxiety? And do you realize that the vast majority of people in the country who develop those same conditions don’t even take any time off work or are able to return after just a short absence? So the people who end up on SSDI are members of a subgroup that has had unexpectedly poor outcomes — including job loss.
You might ask …why does this sub-group have such poor outcomes of conditions that normally don’t cause much work disability at all? It’s logical to assume that these people had the most severe cases of back pain or depression and so on, but in most cases there’s actually no objective data to support that idea. For every person now on long-term disability there are others who started out with the exact same condition, but are still working. From the strictly medical point of view, they looked identical at the beginning. What is different is the way the illness episode unfolded in the two groups: what happened; how others talked to them and treated them; the decisions they made about the best way to manage this life challenge; the effectiveness of the medical treatment they received; the other kinds of support they got and the opportunities that were or weren’t available.
My personal hope is that … more employed people who are dealing with new injuries or illnesses are going to get what they need at the right time to avoid needless impairment work absence, job loss, withdrawal from the work force, and long-term reliance on disability benefits — which really means a life of poverty. That would be good for them, for the tax payers, and for our society as a whole.
Now that these issues are in the spotlight …. It is time for policy makers, employers, healthcare providers, health and disability insurers, other service providers, and affected individuals to start talking together about solutions — and then do their part to make those things happen.
For the last three years, Mathematica‘s policy researchers Yoni Ben Shalom, David Stapleton, and I have been collaborating in the SAW/RTW Collaborative sponsored by the Office of Disability Employment Policy in the US Department of Labor. On September 13, 2016, Mathematica held a forum and webinar during which several speakers presented some actionable policy options that can improve outcomes and prevent needless work disability.
If you want to go deeper … Read my short Work Disability Prevention Manifesto by downloading it from the “Current favorites I’m Sharing” section on my blog homepage. Or you can look at / listen to the recording of the SAW/RTW Collaborative’s September 13 forum/webinar.. Some of the ideas presented by the policy researchers came from surprising angles — and were quite creative / innovative!