My report on Establishing Accountability to Reduce Job Loss After Injury or Illness (commissioned by the US Department of Labor’s Office of Disability Employment Policy) was originally conceived as a simple effort to lay out the rationale for adding work and participation in life to the list of positive health outcomes. (I suspect that I was asked to write it because they thought a physician like me would focus on medical practitioners and the healthcare delivery system.)
Almost immediately, it became obvious to me that in order to make a solid contribution to the on-going public dialogue about health outcomes, the paper would have to explore the meaty issues of explicit expectations, accountability, metrics, credible data, rewards for best practices, and incentives for both participation and performance.
Soon after that, the absurdity of discussing expectations and accountability for the healthcare system alone became obvious —because organizations in other sectors of society play a role in the SAW/RTW process, each of which has enough discretionary power to support or thwart it.
Thus, over time, the purpose of the paper shifted to answering this question: What has to happen in order to engage the professionals at the front-line — the ones who work directly with affected individuals and make discretionary decisions about how much effort to make and for what purpose — so they start making a real effort to help people stay employed?
Who are those front-line professionals?
(1) Healthcare professionals. Most of us view our purpose as making accurate diagnoses and providing appropriate treatment. We are generally not trained to assess work capacity and prevent work disability. Yet our opinions about work have considerable weight under law, regulations, insurance policies and traditional business practices. We generally don’t spend much time and energy thinking about issues outside the exam room.
(2) Workplace supervisors or HR professionals. Their focus is the business of the organization, producing its goods or delivering its services,as well as abiding by company policies and applicable laws. They can decide how much effort to make to help the employee stay at work and keep their job. With rare exceptions, they are neither aware of the preventable nature of most work disability, nor are they trained how to negotiate and arrange stay at work or return to work plans, identify alternative temporary tasks or reasonable accommodations. And they are not incentivized to do so.
(3) Claims/benefits administrators. Their focus is administering the benefit programs correctly, establishing eligibility, compensability, meeting deadlines, making payments, and other requirements. In between these duties, they decide how much effort to make to help the beneficiary/claimant. Like the workplace professionals, with only rare exceptions, they are neither aware of the preventable nature of most work disability, nor are they trained how to negotiate and arrange stay at work or return to work plans, identify alternative temporary tasks or reasonable accommodations. And they are not incentivized to do so.
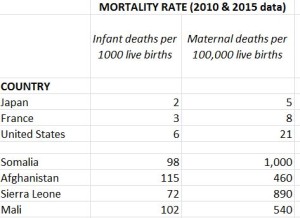
Job loss is the third worst outcome of an injury or illness
As I thought about these players and those who influence their behavior, the biggest realization dawned more slowly: job loss is a potentially devastating secondary consequence of a health-related employment disruption or a failed SAW/RTW process — because it often leads to permanent withdrawal from the workforce. In fact it is the third worst outcome of a health condition, the other two being death and loss of limb or core functions like sight and hearing.
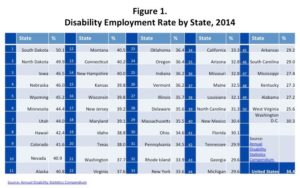
Yet we have not seen it that way. Unlike death and serious injury, job loss is generally not noticed. It’s actually a hidden outcome. The frequency with which it occurs can only be estimated indirectly — because it is untracked and thus invisible. When someone loses their job due to long-lasting illness or injury, they often end up leaving leave the workforce permanently, becoming dependent on public benefits programs like SSDI.
Some years ago, a senior Social Security Administration official commented to me that SSDI is the largest insurance fund IN THE WORLD and yet it has no risk management program, no loss prevention program. Private sector insurance companies view these as core functions of their organizations. They know they must identify and take steps to reduce risks and mitigate losses in order to meet their responsibilities and stay solvent.
In my view, government should be likewise obligated to take steps to protect SSDI (and the taxpayers who fund it) from the economic consequences of the dysfunctions, inadequacies and gaps in the upstream social structures and programs — because their failures end up on public benefit programs.
Government will make a major contribution to reducing demand on SSDI by:
(1) establishing policy that job loss/withdrawal from the workforce is a very unfortunate outcome of a health problem and should be avoided whenever possible,
(2) enabling all parties to see more clearly when it happens by requiring reporting of these events; and
(3) establishing consequences of some sort when involved organizations are non-responsive (negative incentives such as financial penalties, loss of privileges, or public exposure) or do take appropriate action (positive incentives such as credits, privileges, or favorable publicity).
This combination of outcomes visibility and accountability should then start to shift how parties in the private marketplace choose vendors and suppliers.
How will things look different when there IS real accountability for job loss?
Implementing the broad range of actions recommended in the Establishing Accountability report will require a significant long-term effort because of their comprehensive, complex, and varied nature. Taken as a whole, these actions have the potential to create truly transformational change.
Success will mean that more workers living with adult-onset chronic conditions and impairments (acquired disabilities) will be able to stay fully and productively engaged in their own personal, family, and community life; protect their household’s standard of living; remain economically self-sufficient contributors to their local area economy; and avoid dependency on government programs—which will in turn protect their future health and well-being and improve their children’s future prospects. At the national level, success has the potential to stem the tide of declining labor force participation, lighten taxpayer burdens, and bolster the nation’s social fabric and the vitality of the economy. All in all, the initiatives proposed make good use of limited government resources.
The ultimate success of the initiative will hinge on the ability of Federal policy leaders and supporters to create and sustain real multi-stakeholder buy-in and enthusiasm for achieving the future vision described in the paper. A good next step is for the federal and state governments to decide whether and where to start. It will take time and effort to achieve consensus among key stakeholders that this kind of initiative is necessary, timely, and deserves priority for person-power and funding. Once that preliminary groundwork is laid, more detailed planning work can get underway.
Whoever you are, I hope you read the Establishing Accountability paper and agree that change and action is needed. If my suggested recommendations spur you on to creative thinking, you do NOT need to wait for the government to act. You can start factoring these issues into your decisions about who to collaborate with now.
Like this:
Like Loading...