October 9, 2015
A Health & Work Service could prevent or reduce impairment/disability
There is definitely an opportunity to make a positive difference BIG ENOUGH to make the expense and effort of developing, launching and delivering a nationwide community-focused Health & Work Service (HWS) worth it — in my opinion. (Our proposal for establishing the HWS was among 12 ideas selected for development as part of the Committee for a Responsible Federal Budget‘s SSDI Solutions Initiative on Capitol Hill.) There are two main reasons why this opportunity exists.
First reason: Years of research have shown that some of the unfortunate secondary consequences of illness and injury — certain kinds of impairment and work disability — CAN sometimes be prevented or reduced. This is particularly true in people with the most common chronic musculoskeletal conditions (MSK) especially low back pain, and the most common mental disorders (CMD) like depression and anxiety. And research has also shown that intervening early in the unfolding of an injury or illness episode can have a very favorable impact on the long-term outcome.
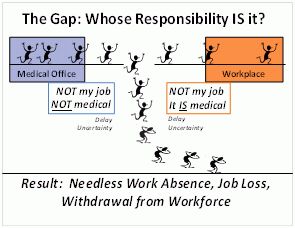
Second reason: Millions of workers in America fall through the cracks in our society because they have no access to services or expertise that might protect them against job loss after injury or illness, or they experience service failures. Many of them work for employers that do not offer health or disability insurance, or that are excluded from the requirement to buy workers’ compensation insurance. Many work for small companies that are exempted from the Family Medical Leave Act which protects jobs for 12 weeks when employees have health problems, or the Americans with Disabilities Act which requires employers to make reasonable accommodations for employees with disabilities. In addition, there are many people who are the victims of neglect or poor decision-making by those with authority over some aspect of their situation. Sub-par employees headed for termination exist among the administrative staff, professionals, supervisors, and managers in every organization, including every medical care facility, workplace, and benefits claims administration organization. Before leaving, each of these sub-par employees has probably had an impact on hundreds of vulnerable workers.
Therefore, it is not correct to assume that all of the people who are now on SSDI due to these common health problems had the worst (most severe) form of their particular MSK or CMD from a biological/pathological perspective, and that nothing could have prevented their entry into SSDI. While undoubtedly true in many cases, it is also likely that a sizable number of them lost their footing in the world of work and ended up on SSDI because of events that occurred in response to their health condition—not the condition itself. Their lives fell apart due to a cascade of adverse secondary consequences of the initial medical problem, and after a time SSDI became the best option for survival.
Remediable or Avoidable Reasons for Poor Outcomes
At the moment when the common health problems of this subgroup of SSDI recipients first started, these people would often have looked very similar to other patients with the same diagnosis and objective clinical findings—but who then experienced good recoveries. This is because the factors that predict poor outcomes (serious impairment and prolonged work disability) as a consequence of MSK, especially low back pain, are not tightly related to either the specific diagnosis or the extent of the pathology. Although less research has been done on factors that predict poor outcomes in CMD, and diagnosis does play a more significant role, there are other important non-medical factors.
Some of the factors that predict poor outcomes are immutable (such as age, past medical history, work history, and geographic location). But other factors are potentially remediable such as elapsed time out of work, uncertainty and distrust due to lack of communication or information, uncoordinated or inappropriate medical care and advice, low expectations of recovery, excessive vigilance, catastrophic thinking, false beliefs, fear of movement, self-limitation, perceived injustice, and lack of employer support. Today, those who handle these situations do not typically look for any of these remediable problems and address them. And none of the professionals involved has been trained to feel responsible for driving the situation forwards towards a good outcome .
The standard medical care process is simply inadequate to help people in these situations avoid poor life outcomes. What is needed is coordinated activity during a fleeting opportunity to address and resolve a set of pivotal issues (both medical and non-medical) around the time the condition starts interfering with work—issues that will set the situation off onto the right or wrong path.
The first few days and weeks after onset are an especially critical period during which the likelihood of a good long-term outcome is being influenced, either favorably or unfavorably, by some simple things that either do or do not happen during that interval. It is the optimal window of opportunity to improve outcomes by simultaneously attending to the worker’s basic needs and concerns as well as coordinating the medical, functional restoration, and occupational aspects of the situation in a coordinated fashion.
The best opportunity for basic intervention appears to last about 12 weeks or three months, although some data shows it ending by 6 months. Many studies have show that a modest set of simple services—that embody an immediate, systematic, pro-active, integrated, and multidimensional approach—can mitigate the potentially destructive impact of common injuries, illnesses, and chronic conditions on quality of life among the working population.
In summary, the way a health-related episode that disrupts work unfolds over time in all dimensions—biological, psychological, social, and economic—can have a big impact on the outcome. Events that occur can either mitigate or aggravate existing risk factors in the situation, leading to better or worse outcomes. There are usually many opportunities to actively influence the course of events immediately after onset of a health problem (and many fewer opportunities later on), but today there are few resources devoted to finding and exercising these opportunities. Most of the current attempts to steer situations to a better outcome are made long after the best opportunities have passed by.
If you’d like the references for the research mentioned above, get a copy of our full report when it is published by the CFRB later this month (electronically) or in January (in print).
Bottom line: If you agree that the USA needs a community-focused Health & Work Service, contact your Congressional representative, tell them you like our proposal and recommend that it be included in the 2016 SSDI reform legislation package. Or even better yet, take a grass-roots approach. Team up with other like-minded people to see if a local charity or foundation will fund your efforts start a HWS in your own community!